Hospitals and health systems across the country are reexamining their clinical service line strategies and operations in response to the shift from volume to value. In addition to population-based and episode-based payment reforms initiated by public and private payers, providers are challenged by mergers and acquisitions, clinical integration, consumerism and price transparency. Strengthening clinical service line strategies and capabilities are critical approaches to addressing these many challenges.
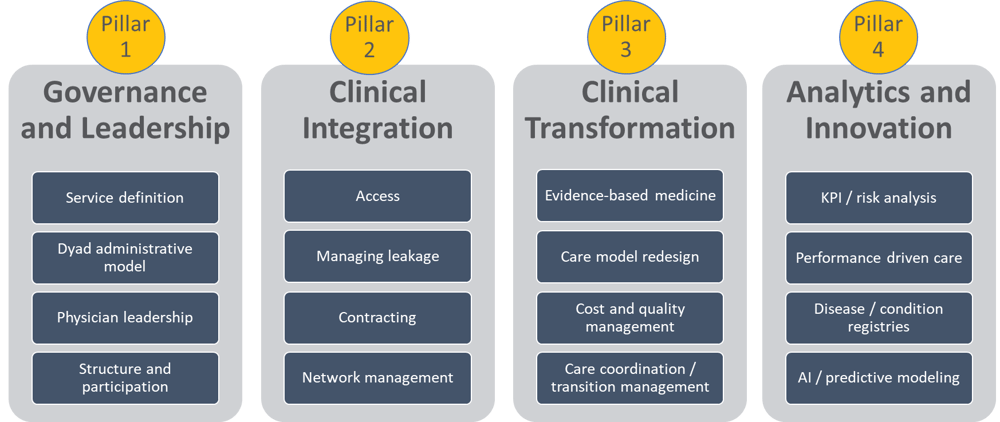
This post is the first in a four-part series where we introduce the pillars of success for clinical service lines: Governance and Leadership, Clinical Integration, Clinical Transformation, and Analytics and Innovation.
The Four Pillars of Clinical Service Line Success
In this post, we address pillar one: Governance and Leadership.
Service Definition
Service line development and optimization begin with deciding which services are in and, as importantly, which are out.
For example, a cardiac service line would clearly include cardiac imaging, heart failure, coronary artery disease, arrhythmia, heart valve problems, and treatment of heart attacks. Depending on size and scope of the service line development, some organizations might exclude thoracic, pulmonary, and stroke care as those could make better sense as part of oncology or neuroscience service-line structures.
Although all medical care affects other medical care, creating effective service line organizations requires setting boundaries in order to manage effectively and efficiently.
Dyad Administrative Model
To accomplish the goals of alignment, improved quality, and reduced costs, service line leaders need to nurture and build relationships among the members. A successful team often includes a dyad of a physician and an administrator to lead development and execution of clinical, operational, and cost improvement processes.
Pairing a physician and administrator requires effective communication between the two top leaders. One or the other may be designated the chief executive officer. If done well, this structure can lead to improved trust and commitment among all the stakeholders.
Most importantly, service line leadership must be independent enough to be able to innovate and develop creative solutions as challenges inevitably arise.
Physician Leadership
Active involvement of physicians should not stop with the dyad model. Physicians providing care throughout the service line should be actively involved across all the four pillars.
Key areas of physician involvement will be described in throughout this four-part blog series.
Many hospitals and health systems working on service line development are also part of a clinically integrated network (CIN), and so strong physician leadership becomes even more important to coordinate services across these programs. As networks evolve to develop specialty physician performance measures and service line integration, CINs without strong physician leadership risk missing their goals for improving quality and costs and may face scrutiny from payer partners and the FTC.
Ideally, each service line integration opportunity will have its own unique governance group to oversee detailed operations. For example, if an organization elects to participate in the program for major joint replacement of the lower extremity, the corresponding governance group could consist of orthopedic surgeons and support staff. These governance bodies can be either existing value committees or new groups created specifically for the service line. Either way, physician members should have equal voting rights.
All decisions that involve service line optimization or care model efficiency should be made with strong physician input.
Structure and Participation
Once an institution has defined the clinical programs to be managed in a specific service line, identification of the appropriate providers for participation is the next step.
Provider participation in an institution is often defined by the goals or value that the organization is trying to accomplish. For example, health systems trying to reduce leakage and improve access may only need a group of physicians and administrators responsible for improving processes and managing referral sources.
However, as many institutions begin to use the service line structure to manage payer contracts that include bundled payments, quality metrics, or total cost of care, participation may need to be much broader and, in fact, may look like a specialty network. In this case, the service line network will include providers from across the clinical services, including physicians (primary and specialty), acute care providers, ambulatory providers, and post-acute providers. A larger, more complex network of care may also need a separate or defined organizational structure.
Service line structure can be formal or informal and usually takes form in order to meet contractual requirements. For example, an institution may include employed and affiliated network members in a value-based contract and therefore may need a formal structure to share savings or incentive payments with independent physicians or institutions. Under current regulations, these kinds of payments may only be made to an independent organization like a CIN, an IPA, or some formally structured LLC. Any shared incentive must be distributed to the affiliated organization, which must have an explicit distribution methodology.
Service line organizations that do not intend to distribute value-based contract payments or that have an entirely employed or owned network of providers and institutions do not need to formalize the organizational structure. These organizations may operate a service line as a department rather than a separate business unit.
In summary, clinical service lines should prioritize governance and leadership as the first pillar of success in value-based contracting. This includes service definition, dyad administrative model, physician leadership and structure and participation.
Parting Thoughts
Most patients don’t understand the health care system at all, much less think about it in terms of sophisticated organizational structures. Organizing care around service lines is designed to address patient confusion or uncertainty by coordinating the efforts of medical professionals all along the continuum of care – from access to diagnosis to treatment to evaluating outcomes.
Patients typically come to the health care system when they are most vulnerable and in need of help and guidance. Effective service line structures organize the care for patients, so they don’t have to organize it for themselves.
Our second blog post in this four-part series will discuss pillar two: Clinical Integration, including access, leakage, contracting and network management.



Share this: